Skin necrosis is uncontrolled skin cell death. Dead tissues can’t revive, but with appropriate treatment, it’s possible for skin as a whole to heal.
Skin Necrosis: Causes, Symptoms & Treatment
In an average year, between 500,000 – 800,000 Americans experience necrosis of skin (and neighboring tissues) due to critical limb ischemia (CLI). The complication affects between 25% and 40% of CLI patients annually.
And they’re not the only ones to deal with skin necrosis. Every year, just over 1.3 million adults in the U.S. develop gangrene—another type of skin necrosis— as a complication of peripheral artery disease (PAD). That’s 16.7% of the 8 million Americans dealing with the condition.
Necrosis can also result from injuries, infections, and wound healing complications. Learn more about the condition with this guide. Unpack what skin necrosis is, how it works, and what to do about it.
Understanding Skin Necrosis (Overview)
Skin necrosis is a complex diagnosis. To understand it, learn about what it is, key signs and symptoms, and what causes the condition.
What Is Skin Necrosis?
Necrosis is pathological cell death. Unlike planned cell death within the body’s natural cycles, necrosis is cell death that’s widespread in tissue, uncontrolled, and irreversible. The cells’ membranes are destroyed during necrosis.
According to The Cleveland Clinic, “Necrosis is the death of the cells in your body tissues. Necrosis can occur due to injuries, infections or diseases. Lack of blood flow to your tissues and extreme environmental conditions can also cause necrosis.”
Skin necrosis is uncontrolled death of skin cells throughout layers of skin tissue. It happens when an injury, condition, or infection prevents blood and oxygen from getting to that part of the skin.
Signs & Symptoms of Necrotic Tissue
The key sign of most types of skin necrosis is a change in the skin’s color, texture, and sensations.
In the earliest stages of necrosis, skin may turn blue or pale. As it loses oxygen, it may become green, dark red, dark blue, or black.
Necrotic skin will likely feel cooler to the touch than surrounding skin. It may become firm, hard, or “crumbly.”
Affected skin often feels different than healthy skin. It may feel extremely painful, much more severely than the pain someone feels from a similarly-sized bruise. On the other hand, skin can also feel painless, tingly, or numb.
Skin tissue damage and infections associated with necrosis also have symptoms. These can include:
- Immunological reactions on skin
- Visible blisters
- Swelling
- Sores
- Subdermal cysts
- Skin cracks oozing pus
- Widespread bruising
- Flu-like symptoms
- Fever
- Chills
- Aches
- Cough
- Rapid heartbeat
- Bleeding
- Coughing up blood
- Blood in urine or stool
- Bleeding from gums
Underlying Causes & Risk Factors
Skin tissue necrosis is the result of skin loosing access to blood or oxygen. Injuries, infections, and autoimmune conditions affecting blood vessels are the most common underlying causes of this loss.
Medical conditions that affect blood vessels increase a person’s risk of developing necrosis. Common conditions include:
- Diabetes
- Peripheral artery disease
- Raynaud’s Syndrome
- Vasculitis
The infectious illnesses most likely to cause necrosis of the skin are Tuberculosis, Histoplasmosis, Syphilis, and C. diff.
5 Notable Types of Skin Necrosis
Skin necrosis is categorized by how skin is affected as tissues die. There are five types of necrosis than can affect the skin. Medical professionals further classify one type, gangrene, into three subtypes.
1. Caseous Skin Necrosis
Caseous necrosis causes painful “crumbly” lesions on the skin. The dead skin had a “cheese-like” texture, and holes form in the skin tissue. It’s typically caused by a bacterial infection like tuberculosis.
2. Fibrinoid Necrosis of Skin Tissue
Fibrinoid necrosis of skin tissue is when the fibrin in small blood vessels collapses, cutting off the blood’s path to that part of the skin. It’s typically caused by autoimmune conditions that cause white blood cells to attack fibrin cells in confusion.
3. Gangrene
Gangrene is the most common type of necrosis to affect skin tissue. It’s a medical emergency, as it involves bloodflow being cutoff from a broader section of skin than is typically affected by fibrinoid necrosis.
In a resource from its medical library, The Cleveland Clinic details three gangrene subtypes most likely to affect the skin.
“Dry gangrene. This is when blood can’t reach a certain area of your body, but there’s no infection. Your skin will feel dry to the touch (no open blisters or pus). Plaque buildup in your arteries (atherosclerosis) is commonly responsible for dry gangrene.
Wet gangrene. This is disrupted blood flow along with a bacterial infection. Blisters that release pus (the “wet” factor) form on your skin. Wet gangrene spreads quickly to nearby tissues.
Gas gangrene. This bacterial infection destroys your soft tissues and blood cells. Bacteria quickly multiply in your muscle tissue, forming toxins and releasing gas. The infection spreads fast and can become life-threatening within hours of symptom onset.”
4. Liquefactive Necrosis of the Skin
Liquefactive necrosis is skin tissue with cells that have liquified as they died. It typically results from chemical burns or fungal infections, which can cause skin cells to lose their structure.
5. Fat Necrosis
Fat necrosis is one of the rare types of necrosis that isn’t that dangerous. It happens when fat cells in a particular cluster die, due to an injury.
The necrotic cells form a hard lump under the skin, and the skin may look red or brown. Fat necrosis clusters typically resolve into oil cysts, and the body usually heal them on its own.
Skin Necrosis Treatment In 6 Steps (Best Practices)
Treating skin necrosis varies, depending on the individual affected and the underlying cause. While not every step on this list is needed in each case, they’re all broadly applicable.
1. Antibiotic / Antimicrobial Treatment
Antibiotics, antivirals, or antifungals should be administered as soon as possible to address any underlying infection. Depending on the condition and how far its spread, medications may be given intravenously, orally, topically, or in some combination.
Getting the correct diagnosis is key. The right antimicrobial will stop the infection. While it cannot revive stage three necrotic skin, it can prevent remaining viable tissues from worsening.
2. Debridement
Any skin that’s reached the necrotic tissue stage needs to be safely removed.
Debridement removes necrotic tissue from the viable skin and wound bed with precise tools. Enzymatic or biological tissue breakdown, surgical removal, and debriding dressings are the most effective options.
One safe, clinically effective option is Medihoney Paste Honey Dressing. Once applied, it changes the internal, physical environment of the wound, triggering autolytic debridement.
In essence, Medihoney naturally draws the body’s own, innate enzymatic fluid to the dead tissue. The necrotic skin is broken down to liquid, and pushed out into the dressing.
This type of debridement is more appropriate for some wounds than others. Be sure to work with a doctor to determine the best option for your condition.
3. Wound Care
Removing necrotic skin leaves a wound. Wound care helps the wound close and heal, empowering new healthy skin to grow in place of the now-removed tissue.
Wound care may involve therapeutic dressings designed to optimize the healing environment. To learn more about available dressings, jump to “Best Dressings For Necrotic Wound Care.”
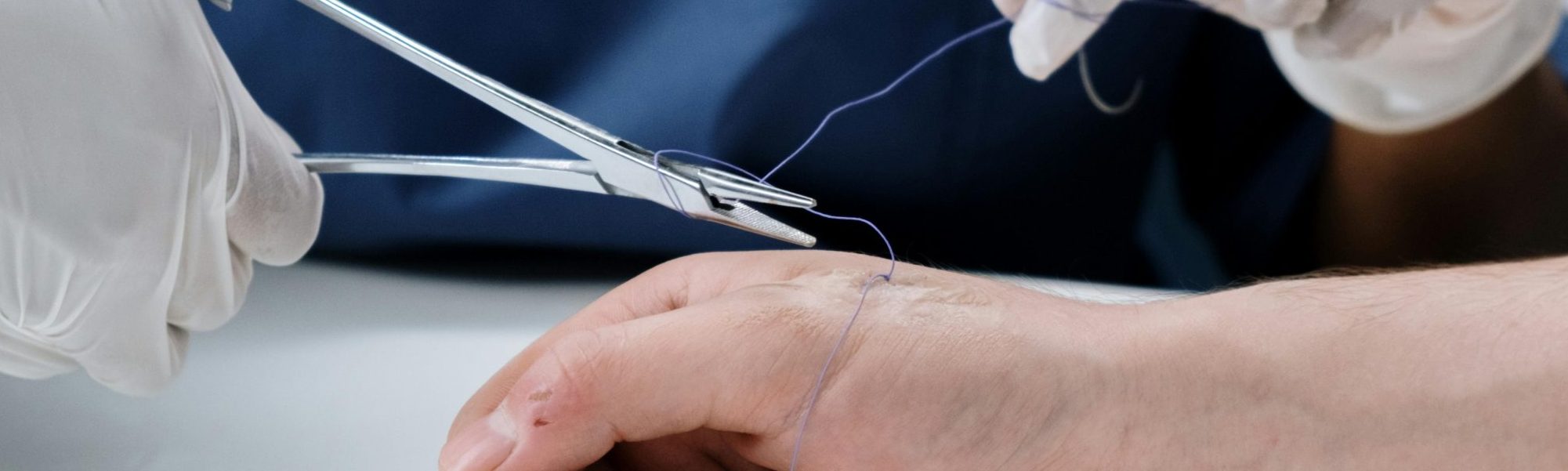
Severe wounds may require sutures or skin grafts to fully heal.
4. Specialized Wound Care & Tissue Treatment
Two specialized therapies can be helpful when treating necrotic skin wounds.
Hyperbaric Oxygen Therapy (HBOT)
When the healing skin and tissues are damaged, and partially or wholly ischemic, Hyperbaric Oxygen Therapy (HBOT) may be integrated into wound care. HBOT pumps 100% oxygen in a pressurized chamber. The patient enters and breathes the pressurized oxygen, typically for 30-120 minutes.
The HBOT session increases the oxygen level in the patient’s blood. The increased oxygen-richness can compensate for decreased vascularization, significantly speeding the renourishment and revitalization of ischemic cells. This, in turn, dramatically accelerates wound healing.
Negative Pressure Wound Therapy (NPWT)
Negative pressure wound therapy (NPWT) is also a common integration during skin necrosis treatment—particularly is the wound is an ulcer or is chronically non-healing.
NPWT uses negative pressure (i.e. suction) to remove fluid and bacteria, while keeping healing cells and blood flowing. In one recent study, “negative pressure therapy was applied to 39 deep pressure ulcers covered by soft necrotic tissue.” The experiment’s results were phenomenal.
The study’s leads concluded, “All of these wounds showed clear wound beds within only 1 month. All of the wounds were successfully cured…[NPWT is] one of the top choices for the management of non healing deep pressure ulcers covered by soft necrotic tissue.”
5. Revascularization / Surgical Blood Flow Repair
Revascularization helps return blood flow to ischemic and viable tissues, and any other region at risk. Treatment might stimulate regrowth of damaged blood vessels, widen blood vessels, or surgically bypass barriers blocking flow.
6. Addressing Risk Factors & Treating Related Conditions
Necrotic skin tissue treatment should include measures to prevent repetition. For most, this means treating any conditions that increase a person’s risk of skin necrosis. Effective, ongoing treatment for diabetes, heart disease, or vasculitis must not be overlooked.
Best Dressings For Necrotic Wound Care
When treating wounds resulting from skin necrosis, or wounds with necrotic tissues, certain types of dressings can aid healing.
Collagen Dressings
Certain dressings offer scaffolding support, which is particularly useful after removing a decent-size area of necrotic skin.
For instance, BIOPAD Collagen Dressing incorporates Type I collagen, which regrowing skin tissue uses as scaffolding. It offers extra support, spurring new tissue formation.
Simultaneously, it draws excess fluid out—preventing buildup of lactic acid, slough, or pus that can stall healing.
Transparent Dressings To Monitor Healing Progress
For wounds covering a smaller area, the Solventum 3M Tegaderm Transparent Film Dressing is a great option. The transparency makes it easy to track the wound’s healing progress, which is key.
Catching signs of potential re-infection or ischemia early is vital to complete recovery from skin necrosis. If healing gets off-track, without swift intervention a post-skin-necrosis wound can become chronic. A transparent, breathable, long-term-use dressing simplifies proactive prevention.
Hydrophilic Dressing For Eschar Management
A wound might have dry remnants of necrotic tissue (eschar), even after the bulk of the tissue is removed. In those cases, an autolytic gel dressing can help.
The Triad Hydrophilic Wound Dressing is a zinc oxide-based paste with soothing ingredients. Applied to a wound, it creates a gel that absorbs excess exudate and generates a moist healing environment.
The absorption jumpstarts an autolytic debridement process, pushing dry eschar out from the wound bed and into the gel.
Product Solutions

BIOPAD Collagen Dressing
Formulated with Type I equine collagen, BIOPAD is a primary dressing specifically created for helping treat challenging wounds. Type I collagen helps with scaffolding, encouraging

Tegaderm Transparent Film Dressing – Picture Frame Style
3M Tegaderm Transparent Film Dressings consist of a thin film backing with a hypoallergenic, latex-free adhesive that gently, yet securely, adheres to skin. Tegaderm transparent

Triad Hydrophilic Wound Dressing
Triad hydrophilic wound dressings use a zinc oxide-based paste to absorb low to moderate amounts of fluid. At the same time, the solution once applied

Medihoney Paste Honey Dressing
Packaged in a tube, MEDIHONEY® Paste is made of 100% Leptospermum honey and free of gelling agents. This results in a thinner, more runny consistency
Top Related Brands
Related Videos
Related Blogs

How to Manage a Highly Exuding Wound
Exudate management is a key factor in treating patients with hard-to-heal wounds. Exudate plays an

The Methods of Wound Debridement
Chronic wounds are, by definition, difficult to heal. An entire area of medical specialty is

Why is My Wound Not Healing?
You may wonder, “why is my wound not healing?”. Generally, wounds can heal alone, especially