Stoma prolapse is a potential complication risk faced by ostomy patients. Yet, the nature of the complication can be unclear at first. Here’s what stoma prolapse is, how it’s diagnosed, and treatment options for the condition.
What Is Stoma Prolapse?
Stoma prolapse is a complication that affects 1.7% to 25% of ostomy patients. Colostomy patients are more likely to experience prolapse than ileostomy patients, and loop stomas result in prolapse more often than end stomas.
To understand the nature of stoma prolapse in detail, it’s important to first understand what a stoma is.
Stoma Definition
The National Institute of Health defines “stoma,” as “A surgically created opening from an area inside the body to the outside.”
Most stomata are openings to divert bodily waste out of the body artificially, when a person’s organs cannot process that waste safely. Common medical stoma types include:
- Small intestinal stoma (ileostomy)
- Large intestinal (colostomy)
- Urinary stoma via intestine (urostomy)
- Stomach stoma to insert feeding tube (gastrostomy)
The frequency of stoma complications, including stoma prolapse, varies by stoma type and patient risk factors.
Stoma Prolapse Definition
Stoma prolapse is an “abnormal protrusion” of the stoma site organ from a person’s body, through the stoma opening.
As a medical complication, stoma prolapse is further defined by location.
What Is Intestinal Stoma Prolapse?
Intestinal stoma prolapse is a complication of an ileostomy, colostomy, or urostomy, where the intestine pushes through the stoma.
The medical journal Annals of Coloproctology defines intestinal stoma prolapse as “an expansion of the intestine from the stoma.” Coloproctologists further emphasize that it’s “a full-thickness protrusion of the bowel through the stoma site…diagnosed when the stoma increases in size after maturation, requiring a change of appliance or surgical treatment.”
Intestinal Stoma Prolapse: Simple Definition
Plainly, the intestine shifts, elongates, or expands. The bowel then partially passes through the surgical opening. It visibly extrudes from the body. Typically, it widens the stoma.
What Is Gastric Stoma Prolapse? (Prolapse Through Gastronomy Tract)
Gastric stoma prolapse is also called “strangulated gastric prolapse,” “g tube prolapse,” and “prolapse through the gastronomy tract” in medical literature. Like its intestinal counterpart, gastric prolapse is a protrusion of an organ through the stoma.
Gastroenterologists define gastric stoma prolapse as, “a full-thickness protrusion, or evagination, of the stomach through the abdominal wall, resulting in exposed gastric mucosa.”
Gastric Prolapse Is Rare
Unlike intestinal stoma prolapse, gastric prolapse is an acute medical emergency. It’s also much rarer: only 1.2% of pediatric patients with gastronomies experience prolapse complications. For adult patients, the condition is even rarer—infrequent enough that no statistics are available.
Because gastric stoma prolapse is so rare, this condition page focuses on intestinal stoma prolapse.
Is Stoma Prolapse An Emergency?
Stoma prolapse isn’t usually an emergency. However, if a stoma prolapse is accompanied by certain other symptoms, you should go to the ER. Emergency stoma prolapse symptoms include:
- Sharp abdominal pain
- Bleeding
- Discoloration
- Vomiting or severe nausea
- Inability to pass stool
- Loss of appetite
Even when a stoma prolapse isn’t an emergency, it’s important to inform your healthcare team when it happens.
What Are The Signs of Stoma Prolapse?
The key sign of a stoma prolapse is visible external intestine. If you can see your intestine pushing through the stoma, that’s a stoma prolapse.
Other symptoms include peristomal skin irritation, pain, and difficulty adhering the ostomy bag.
Types of Stoma Prolapse: Symptoms and Severity
Stoma prolapse is medically classified by intestine movement and prolapse severity.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9650348/
Fixed Vs. Sliding
Fixed prolapse is a condition where the prolapse (intestine extrusion) remains fairly constant. The intestine doesn’t easily or naturally slide back into its internal position.
In contrast, sliding prolapse is a condition where the intestine intermittently passes through the stoma opening, and then slides back inside.
Fixed prolapses often require surgical intervention, while sliding prolapses are often manageable without surgery.
Severity (Grades)
The severity of a stoma prolapse is related to its degree of protrusion, the presence of other symptoms, and any restrictions on activities of daily living (ADL) imposed by the prolapse.
Grades are standardized in The Common Terminology Criteria for Adverse Events Classification.
Grade 1
A grade 1 stoma prolapse has no accompanying symptoms. It’s “easily reducible,” meaning it’s relatively easy to manually push the extruding intestine back into its correct place. n
Grade 2
A grade 2 stoma prolapse shows “some recurrence after manual reduction; local irritation and stool leakage as stoma appliances are difficult to fit; and instrumental activities of daily living [are disrupted].”
This type of stoma prolapse doesn’t require surgical treatment, but it likely needs specific medical intervention to reduce it. Peristomal skin injuries or irritation may also need treatment, and stoma appliances may need to be resized or adjusted.
Grade 3
A grade 3 stoma prolapse is an extrusion accompanied by “high-grade symptoms and the need for elective surgical treatment, with the restriction of ADL.”
When a stoma prolapse involves injury to or strangulation of the stoma, pain, and makes stoma care difficult or impossible, surgical treatment is necessary.
Grade 4
A grade 4 stoma prolapse is the most dangerous. It creates “life-threatening medical conditions caused by the prolapse require emergent treatment.”
Life-threatening conditions caused by stoma prolapse can include moderate to severe bleeding, sharp pain, and signs of stoma strangulation or necrosis.
How Is Stoma Prolapse Diagnosed?
Stoma prolapse is diagnosed by assessing the length of intestine protrusion, its color, and any associated symptoms.
What Are The Best Stoma Prolapse Treatment Options?
Grade 1 and grade 2 stoma prolapses are treated without surgery. Grade 3 and 4 stoma prolapses require surgical intervention.
Non-Surgical Treatment
There are four standard, non-surgical treatment options for stoma prolapse. These include:
- Manual reduction
- Topical osmotic therapy
- Relaxation reduction
- Management and prevention
Which non-surgical treatment is best depends on factors like personal comfort level and the underlying cause of the prolapse.
Manual Reduction (Pressing)
Manual reduction is simply, gently pressing the extruding bowel back inside through the stoma. To reduce pain and swelling, many choose to apply a cold compress to the stoma before or during reduction.
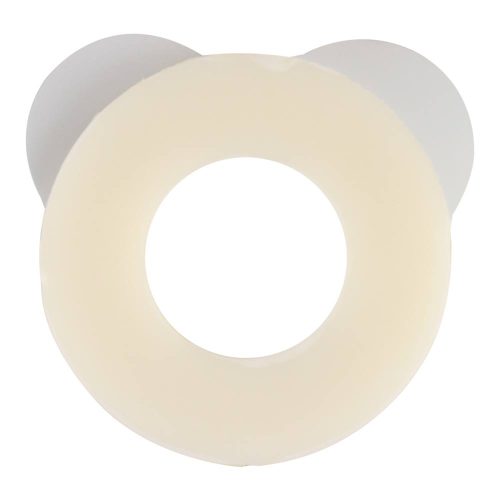
In one case study model, a nurse demonstrated how to use a flexible, cut-to-fit pouch system with a soft convex barrier to aid comfortable manual reduction.
Topical Osmotic Therapy
Topical osmotic therapy is applying an osmotic agent (a substance that absorbs water) to the surface of the extruding bowel, in order to reduce its size. Often, sugar is used.
Pulling excess water from the bowel can bring down swelling. Once it’s smaller, it’s easier to manually reduce the prolapse without injuring the bowel or stoma.
Relaxation Reduction
Relaxation reduction can be done alone if the prolapse is very mild. To reduce the stoma prolapse independently, lie on your back. Rest your hands gently on the stoma. Do not press. Then, systematically relax all muscles in your abdomen, then your back and sides. As your muscles relax, the stoma will gently slide back in.
Management and Prevention
There are plenty of options for managing a prolapsed stoma. And there are tools to prevent its recurrence.
To mitigate the risk of recurring stoma prolapse, consider wearing stoma support garments, such as a support belt or midriff tube.
It’s also wise to talk to your healthcare team about how you might engage in physical fitness safely. Improving your abdominal strength and immune health through exercise reduces the risk of prolapse. Strong abdominal muscles are better able to hold your intestine in place, and a strong immune system can fight certain underlying causes of prolapse.
Surgical Treatment
If you experience a grade 3 or grade 4 stoma prolapse, you will need surgical treatment. Only your doctor can tell you what kind of surgery is appropriate for your care. However, in general, there are three types of surgical interventions for stoma prolapse.
Intestine Fix
To fix the intestine, the surgeon uses a device or implant to firmly secure the intestine inside the body. This prevents it from sliding out of the stoma again.
Shorten Intestine
Surgically shortening the intestine means removing part of the bowel organ (usually something damaged, infected, or necrotic). The resulting intestine is shorter, making it less likely to cross the internal distance to exude through the stoma again.
Repair Stoma Outlet
Sometimes the extruding intestine damages the stoma outlet during prolapse. In that case, surgery is required to repair the opening. In some extreme cases, the stoma will be surgically closed, and a new stoma will be created in a better location.
Heal and Protect Your Stoma With Medical Monks
At Medical Monks, quality ostomy care is our priority. Explore our wide range of stoma care supplies and products available in our online store. If you have questions or need assistance, chat with one of our agents online. Or, call our team at 844-859-9400

The MEDICAL MONKS STAFF brings to the table decades of combined knowledge and experience in the medical products industry.
Edited for content by JORDAN GAYSO.